Volume 5
Happy Wednesday and Pride Month!
The past two weeks have been very busy with a lot of important healthcare news. But don’t worry! I’ve summarized the most important things you need to know.
As always, for deeper dives, click on the hyperlinks in summaries!
1. Finally. Young Children Are Eligible for COVID Vaccines
The CDC and FDA have approved the Pfizer and Moderna COVID-19 vaccines for children ages six months to five years old. Children receiving Moderna will need two shots; kids getting the Pfizer immunization will need three. Physicians are worried the differing courses of treatment will cause confusion and that parents who opt for Pfizer will stop after just two doses. The good news: side-effects for children are short-term and mild, mainly fever and fatigue. There has been no evidence of the rare, but more serious side effects seen rarely in adults, including myocarditis.
So What’s The Big Deal? Vaccinating young children is an important step to curbing viral spread. Yet, for nearly two years, a gap remained. While the initial strains of COVID-19 were found less in children, as the virus has mutated, more children have gotten ill and even died. Parents of smaller children have had a difficult time managing school and childcare shutdowns because their children exist in largely unvaccinated populations. This news should help ease their minds.
So Now What? Get your children vaccinated. The FDA and CDC reviewed mountains of data from Moderna and Pfizer and found the immunizations’ benefits far outweigh any risks.
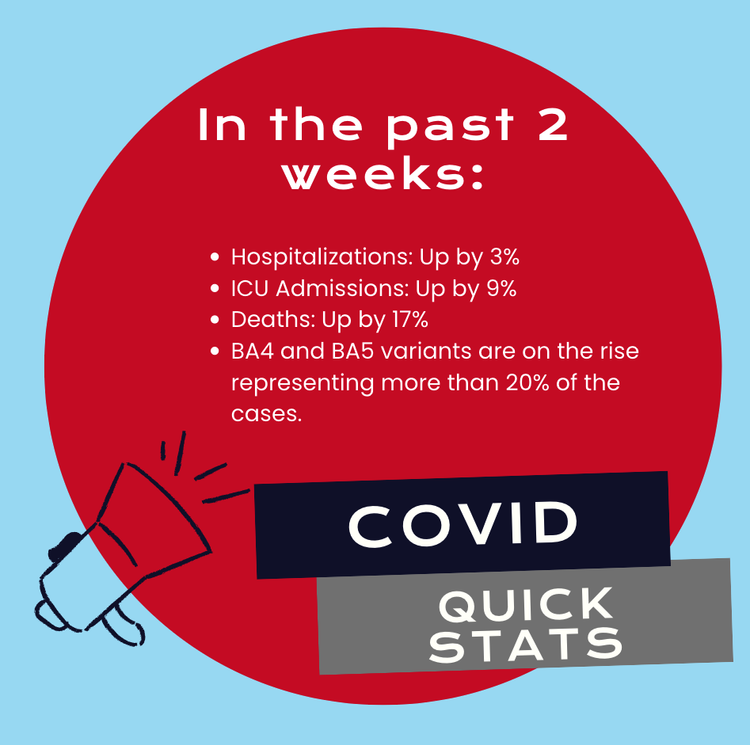
2. Omicron Subvariants Gain Ground in the US
COVID-19 is not gone. And it is mutating once again. According to federal data, the BA.4 and BA.5 sub-variants of Omicron are now responsible for more than one-fifth of U.S. cases, and that number is growing by the day. The good news is the variants do not appear to be any more severe, but they do spread more quickly. With COVID restrictions all but nonexistent and young populations still ineligible for boosters, scientists worry about significant spread and a resurgence in cases once school is back in session.
So What’s The Big Deal? I agree. These new strains appear to evade immunity. Depending on the immune escape, we could see a rise in cases, hospitalizations, and deaths in the mid-to-late summer in the Northeast and then move to other parts of the country. Vaccination and boosters continue to remain the best method to prevent severe illness and death.
So Now What? While new “Omicron” specific vaccines are currently in development, waiting is not advisable. Clinicians should encourage eligible patients to get boosted. And hospitals and clinicians should prepare for another wave of infection.
ABIG’s Covid Quick Stats
3. Monkeypox: What’s In A Name?
The World Health Organization has said the term monkeypox is "discriminatory and stigmatizing” – and inaccurate. The assessment comes after a group of 29 biologists and researchers issued a public statement calling for a new name and arguing the current outbreak has no “clear link to Africa.” The WHO is now working to rename the virus to something like hMPXV. The bigger issue here, though, is that this virus now has been reported in 39 countries, and most of them never saw the disease before.
So What’s The Big Deal? Two things. Monkeypox is not behaving like it has in the past. This could mean greater and faster spread. The window is narrowing for an opportunity to contain the virus. Two, stigma is dangerous and real. It can worsen the spread and foment violence and discrimination against stigmatized groups.
So Now What? Clinicians should follow the virus closely since it is behaving differently than what has been described in the past. Also, clinicians and public health workers should be very cautious about bias which could lead to misdiagnosis. Know the facts, and understand the risks and treatments.
4. Food or Health Care: Older Adults Faced with Dire Choice
Inflation is real and health care inflation is a particular problem. HHS data show out-of-pocket healthcare expenses for adults 65 and older increased 41 percent from 2009 to 2019. Older Americans are feeling the impact. According to a new Gallup survey, more than one-third of adults 50 and over say that they have reduced their food budgets to pay for healthcare. Others are skipping healthcare and medication to pay for food. Women and Black older Americans are the most likely to make cuts. Gallup also found 37 percent of Americans are worried about affording health care in the next year.
So What’s The Big Deal? The result of these inflation-related choices could be worsened healthcare disparities for various communities of color and poor outcomes for low-to-middle income older adults.
So Now What? We all need to take responsibility for this crisis. Clinicians must recognize the out-of-pocket expense burden on patients and identify the most valuable alternatives for equivalent medical care and treatment. Clinical and social work staff must appreciate and understand the financial barriers to care when working with patients. Policymakers need to consider the implications for growing out-of-pocket costs for older Americans.
5. A National Medical Records Database? Doubtful.
In case you missed it, Oracle Chairman Larry Ellison bought the information technology company Cerner for $28 billion. He wants to use the company as a platform to build a national health records database. Even if this dream can become reality, experts say it will take years if not decades because of barriers like lack of coordination among different facilities and health systems and inconsistent technical standards.
So What’s The Big Deal? Physicians, nurses and health policymakers have long understood the importance of integrated health records for patients. Benefits of an integrated system include operational efficiencies, improved patient safety, and reduced costs. The Oracle/Cerner move signals further integration in the healthcare market and more specifically in healthcare IT, but a unified system will take time and even more investment.
So Now What? Wait and see. This is the first time an IT giant has stepped in to try and fix healthcare. Let’s hope more visionaries follow.
6. Yes, Gun Violence Is A Public Health Issue
According to a 2021 U.S. Government Accountability Office report, hospital costs for initial gun injury care totaled more than $1 billion a year in 2016 and 2017 (the latest data available), and costs associated with physicians' fees could add 20 percent to that total. Physicians, policymakers, and other stakeholders are coming together to recognize and elevate the conversation about the mental, emotional, and financial impact gun violence has on the healthcare system.
So What’s The Big Deal? The AMA, ACHE and other physician organizations are recognizing the significant burden gun violence has on the healthcare system and patients. With gun violence now the number cause of death for children, many healthcare advocacy organizations are encouraging the government and others to take a public health approach to “treating” the gun violence problem.
So Now What? Congress is currently crafting a bipartisan bill to hopefully curb gun violence, address mental health resources, and other prevention measures. As of last night (6/21) it appears it will pass the Senate and then on to the House. We will need to see what’s in the final bill to understand where the funding will be focused.
7. Time to Get Excited About SCOTUS 340B Decision? Ehh, Maybe Not.
The U.S. Supreme Court doesn’t issue unanimous rulings very often, but this month all nine justices agreed that, under the Trump administration, HHS unlawfully reduced pharmaceutical subsidies to 340B hospitals. Hospitals had sued the government, and now may be able to recoup billions in drug subsidies. Indeed, the amount affected by the cuts totaled about $1.6 billion each year in 2018 and 2019. Before you get excited, however … recouping funds may prove difficult. Hospital advocacy groups will be working with CMS to determine how the dollars will be reimbursed.
So What’s The Big Deal? The Supreme Court unanimously ruled in favor of hospitals; however, the decision was narrowly focused. While it appears hospitals may be due money for the cuts, CMS already redistributed money to all hospitals included in the Medicare’s outpatient payments.
So Now What? Wait and see. CMS is reviewing the ruling and while some hospitals could see repayments, CMS has made adjustments to payment schedules which could affect their agencies ability to pay back money owed.
8. More than 100 Million Americans Have Healthcare Debt
While older Americans are choosing between food and health care, families are going deeper into healthcare debt. According to a study by Kaiser Health Network and National Public Radio, 100 million people in America, including 41 percent of adults, have health care debt. In the past five years, more than half of U.S. adults said they’ve gone into debt because of medical or dental bills. Policymakers and other stakeholders don’t have visibility into this problem because much of the debt is held on credit card balances, in loans from family, or payment plans to hospitals and other medical providers.
So What’s The Big Deal? This report is additional evidence that the growing burden of healthcare debt is affecting basic choices between food, housing, transportation, and healthcare needs. This results in growing healthcare disparities, reducing healthcare access and worsening overall outcomes.
So Now What? Clinicians must account for the burden of costs as drivers for compliance for medications, access and outcomes. While the Affordable Care Act capped individual out-of-pocket expenses to $8,700, the amount remains too high for most low and middle income Americans. Congress must act.
9. The Biden Administration Is Having A Tough Time Curbing PE’s Influence in Healthcare
Despite the Biden administration’s best efforts, a review of records by KPMG Advisory Services and shared with Morning Consult, found there were 1,145 private equity deals involving health systems, physician practices, nursing homes and disability care in 2021. The deals totaled $18.3 billion. Meanwhile, a federal report found 11 percent of U.S. nursing homes and four percent of hospitals are now owned by private equity firms.
So What’s The Big Deal? Private equity firms have continued to invest more heavily in healthcare, controlling everything from provider staffing to hospitals to technologies and therapeutics. Despite the Biden administration’s efforts to curb some PE’s influence on healthcare, it appears for now, PE will continue to be a major player in the U.S. healthcare market albeit with growing regulatory oversight.
So Now What? Policymakers must understand the role private equity has in healthcare and how value is created (and for whom) value is created
10. Facebook Knows Your Health History?
Big tech is already under intense scrutiny by state and federal lawmakers. Online privacy, antitrust, and the company’s influence on child mental health and well-being all have caught policymakers’ eye. Now let’s add another problem: 33 of Newsweek’s top 100 U.S. hospitals are sending sensitive data to Facebook … without patients’ consent. Former regulators, health data security experts, and privacy advocates say the hospitals may have violated HIPAA.
So What’s The Big Deal? This news is highly concerning. Hospitals are playing fast and loose with privacy laws if third parties (i.e. Facebook) are allowed to receive personal identifiable patient information. While Facebook may not be on the hook for HIPAA violations, hospitals could be. So it begs the question? Why would hospital systems allow for ad-tracking software to be embedded into their websites? Are patients aware?
So Now What? Hospitals must make every effort to protect the private information of patients. Patients and clinicians should be aware of potential privacy concerns with hospital web-based scheduling software.
Thanks for reading the Top 10 Big Deals in Healthcare!
Let’s keep the conversation going! Click on my social media icons below for questions and comments!
Have a wonderful rest of the week!
-Dr. N. Adam Brown
Follow me on social:
Thanks for reading the Top 10 Big Deals in Healthcare and be sure to share with your network: